Aesthetic practitioners are in the privileged position of being able to offer patients treatments for their cosmetic concerns. Many of the changes in the texture and integrity of the skin that signal the passage of time are caused by chronic UV exposure from the sun, which is also a major risk factor for skin cancer. During your assessment, you may encounter suspicious skin lesions, or the patient may ask you to review specific lesions during the consultation. The latter scenario will become increasingly more common with the shortage of face-to-face GP appointments. You may be the first healthcare professional the patient has seen in a long time.
Recent data released by NHS Digital has confirmed that we are in the midst of a skin cancer pandemic. In the years leading up to 2019, there was a rise in the rates of the 3 major skin cancers; basal cell carcinoma (24%), squamous cell carcinoma (19%) and melanoma (27%). The exact cause for this rise is not clear, however, with skin cancer becoming increasingly common, it is important to remain vigilant when assessing patients.
Skin cancers are the downstream result of UV-induced damage to keratinocytes and melanocytes in the skin. Two forms of ultraviolet radiation reach the earth’s surface from the sun. UVA (315- 400 nanometres) is present all year round and penetrates clouds and window glass. It penetrates deep into the skin and interacts with water molecules, generating free radicals that can damage keratinocyte DNA and key proteins. Chronic exposure to UVA is responsible for many of the signs associated with extrinsic skin ageing e.g., freckling, hyperpigmentation, fine lines, and wrinkles. UVB (280-315 nanometres) peaks during the summer months in the UK. It does not penetrate clouds or window glass. UVB radiation causes direct damage to epidermal keratinocyte DNA by inducing strand breaks that can lead to mutations. Sunburn is caused by UVB and is the manifestation of DNA damage. UV radiation is also immunosuppressive, a property that is harnessed by dermatologists to deliver phototherapy. The combination of mutagenesis and immunosuppression creates a perfect storm for the development of skin cancer.
Taking a history
History taking is an information gathering process and asking the right questions will help distinguish lesions that can be safely monitored from those that require consultant dermatologist review. The following questions should be asked when enquiring about a skin lesion:
- Where is the lesion?
- How long has it been there for?
- Is it pigmented?
- Has it changed in size, shape or colour?
- Is it symptomatic (itchy, sore or bleeding)?
- Have you done anything to the lesion?
- Have you had similar lesions in the past?
Risk stratification
Risk factor assessment will help to identify those at increased risk of developing skin cancers. Common risk factors include:
Age
Age is a surrogate marker for sun exposure. Older people are at greater risk of being affected by skin cancer as they have had more UV exposure.
Family history
A strong family history of skin cancer suggests an inherited susceptibility and will put patients at increased risk of developing skin cancer. Some genetic conditions are associated with skin cancer and include: FAMMM (familial atypical multiple mole melanoma syndrome), Gorlin’s syndrome and Xeroderma Pigmentosa.
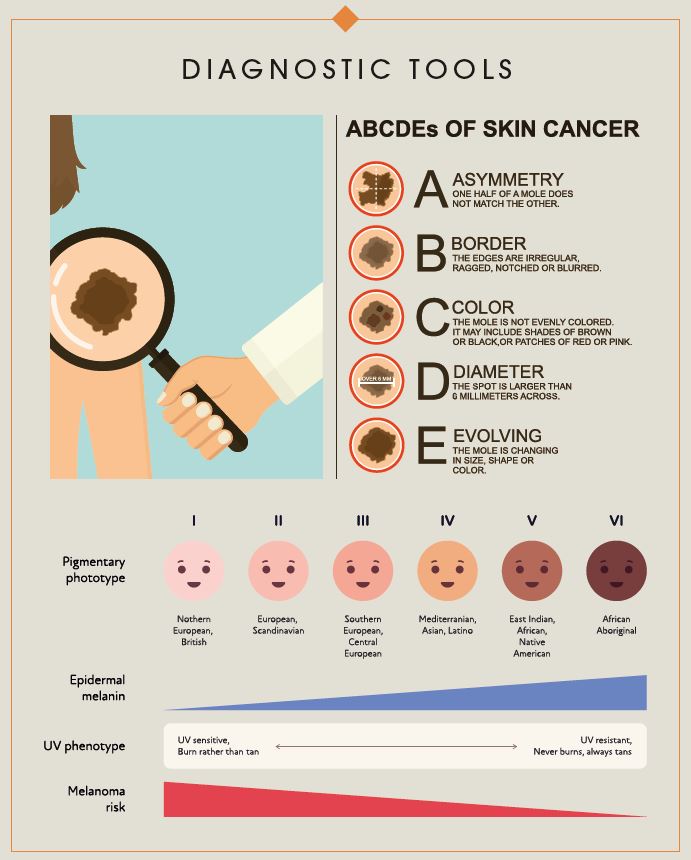
Skin type
The Fitzpatrick scale was developed to describe an individual’s susceptibility to UV radiation. Individuals with Fitzpatrick type I skin are fair skinned with freckles and red hair. They never tan and always burn. Whilst individuals with Fitzpatrick type VI skin have black skin, always tan and almost never burn. The risk of developing skin cancer from UV exposure decreases as you progress along the Fitzpatrick scale. Skin cancer most commonly affects Fitzpatrick phototypes I-III.
UV exposure
This is the major risk factor for skin cancer. Patients who enjoy regular sunny holidays, exhibit sun-seeking behaviours (e.g. sunbathing) and report prior sunbed use, are at increased risk of skin cancer. A history of severe sunburn with blistering is also important as symptomatic sunburn is indicative of DNA damage.
Immunosuppression
One of the functions of the immune system is to identify mutations and trigger programmed cell death to prevent development of cancer. This function is known as immune surveillance and is disrupted by medications that suppress the immune system (e.g., Cyclosporin A, Tacrolimus, Sirolimus, Mycopenolate Mofetil).
Multiple moles (>50)
Melanoma is a skin cancer that arises from new or existing moles. Having more than 50 moles increases the baseline risk of developing melanoma.
Atypical moles
Atypical moles are moles that look abnormal and show evidence of dysplasia at a cellular level. Having atypical moles also increases your baseline risk of melanoma.
Assessing pigmented lesions
The final step in your assessment will be the examination. This can be particularly daunting if you have little prior dermatology experience. The ABCDE framework is a useful tool for assessing pigmented lesions.
Asymmetry- Benign lesions are typically symmetrical. If you draw a line through the lesion, one half should match the other.
Irregular Borders- Benign lesions have smooth, even, regular borders whereas melanoma has an irregular and jagged outline.
Multiple Colours- Benign lesions typically have one colour, whilst melanoma will have multiple colours (black, brown, blue, areas of regression).
Diameter more than 6mm. Benign moles are usually small.
Evolving- Benign moles tend to look the same over long periods whilst melanoma will change in size, shape and colour over weeks and months.
Two or more features are an indication to refer to a consultant dermatologist for further assessment. Dermatologists are able to perform an in-depth assessment, using dermoscopy to review the pigment structure of lesions and identify diagnostic features.
Consultant dermatologists are trained in the diagnosis and management of more than 2000 conditions affecting the hair, skin and nails. We have focused on skin lesions in this article due to the rising rates of skin cancer in the UK and potential implications of late diagnosis. However, you can refer patients with acne, rosacea, eczema, psoriasis or any rash of concern.
Dr Derrick Phillips is a London based Consultant Dermatologist, and he addressed this topic at Wigmore Presents in May 2022. For more information, visit drderrickphillips.com

 Added to basket
Added to basket

 Unapplied Changes
Unapplied Changes